The mysterious nature and high stakes associated with SIDS make it a media magnet. Sensational titles gather social shares - the scarier the article the more the shares. Out of sheer paranoia, parents have started avoiding the most benign child care products, often without understanding the facts about SIDS.
Today we shed some light on the research that has been performed on SIDS. Our aim is to provide you with scientific proof taken from journals and papers on various studies on SIDS. All references are given at the end of this article.
The information in this article has two levels: basic and scientifically in-depth. The basic level is meant for all readers. The scientific support, which details the research and associated conclusions, is provided for the more curious and thorough.
It is our aim to present facts showing no bias and to leave you with enough data to form an informed opinion about this feared phenomenon called SIDS. In order to be unbiased we had to present the facts as they are. If the information provided is too frank for some, we understand and apologize in advance.
In this article we will cover the following:
1) What is SIDS?
2) How SIDS is Diagnosed
3) Known Facts About the Systems Involved in SIDS
4) The Circumstances Under Which SIDS Occurs
5) Prenatal and Post Natal Smoking and SIDS
6) Swaddling and SIDS
7) Sleep Maturity From 6 Weeks to 6 Months
8) Can SIDS be Prevented?
9) References
What is SIDS?
Sudden Infant Death Syndrome (SIDS) is where an infant younger than one year meets an untimely and unexplained death while sleeping.
SIDS occurs when babies do not wake up despite being under life threatening circumstances. Accidental suffocation is a prime example of SIDS. When a baby’s breathing becomes obstructed during sleep, a normal response would be to wake up or adjust position to clear airways and allow breathing. However, in this instance, the victim does not adjust or wake up resulting in suffocation.
SIDS is feared mainly due to its unknown causes. It is feared, because despite decades of research such little is known about why or exactly how infants still die from it. In fact, in the United States, it is the leading cause of death in children between 1 month and 1 year of age. The incidence of SIDS peaks between 2 and 4 months of age and approximately 90% of SIDS deaths occur before the age of 6 months.11
How SIDS is diagnosed
You may ask, ‘if causes are unknown then how are babies pronounced dead due to SIDS’? When the cause of an ailment is known, the diagnosis is direct. To oversimplify, a runny nose may be caused by a common cold or seasonal allergy. That’s a direct diagnosis. However when the cause is unknown, the diagnosis cannot be direct.
SIDS is diagnosed by a process of elimination. In other words, ruling out what the cause of death is not. This investigation includes performing a complete autopsy, examining the death scene, reviewing the clinical history and ruling out other causes before pronouncing the baby dead due to SIDS.
When a baby dies, health care providers, law enforcement personnel and communities try to find out why. They ask questions, examine the baby, gather information and run tests. If they can’t find a cause for the death and if the baby was younger than 1 year old, the medical examiner or coroner will call the cause of death SIDS.
If there is still some uncertainty as to the cause after it is determined to be fully unexplained, the medical examiner or corner might leave the cause of death as “unknown”. Could there anything be more mysterious?
Known Facts About the Systems Involved in SIDS
Despite the mystery surrounding SIDS, studies have show links between SIDS victims and abnormalities in the functioning of the heart, breathing and brain signals related to the process of waking up from sleep - also known as "arousal" from sleep.
Genetics have also been seen to play a role, as there have been cases where some victims of SIDS have had siblings die in the same manner. These preconditions mean that some babies who were SIDS victims could have been predisposed to the syndrome and more prone to SIDS than others.
Before we describe these life threatening circumstances it is important to understand the process of sleep and wakefulness and what parts of the baby’s body, if impaired, may increase the risk of SIDS. This may also help us to better understand the preconditions.
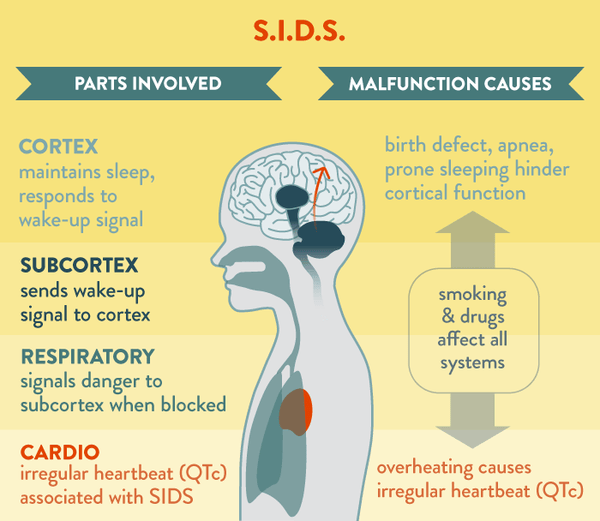
Pioneering studies of scientists and neurophysiologists Pavlov (1928), Bremer (1930), Dempsey (1941) and Moruzzi (1972) explain the parts of the brain that are involved in the process of waking up, or arousal, from a state of sleep. We will use the image above to explain.
The cortex maintains the state of sleep until it receives a signal to wake up. The sub-cortex sends a signal to the cortex to wake up. The waking up is called "cortical arousal". This wake-up signal is called "sub-cortical activation". The sub-cortex detects situations that may hinder our safety and sends an involuntary activation signal to the context requesting it to wake up in order to protect us. The sub-cortical activation may occur in both REM and Non-REM sleep.
However, cortical arousal occurs more during REM sleep than during Non-REM sleep. This is the primary reason why infant sleep consists mainly of REM15 sleep when the autonomous nervous system, responsible for involuntary functions, alerts the brain to wake up when surrounding situations are unsafe or uncomfortable. In REM sleep, a baby may wake up for many reasons; such as hunger, a soiled diaper, stuffy nose or a doorbell.
Now that we understand the process of sleeping and waking up, let us look into the malfunctions of systems that hinder waking up due to abnormalities in the pathways of cortical arousal.
SIDS FINDING #1: INCOMPLETE AROUSAL PROCESS
SIDS victims have shown that even when the sub-cortex signals the cortex to wake up, the cortex does not complete the arousal process by fully waking up. As a result there are fewer cortical arousals and more-frequent subcortical activations.
These findings suggest an incomplete arousal process in victims of SIDS. So victims of SIDS, who were found to be in life threatening situations, did not wake up to call attention.
SIDS FINDING #2: PROLONGED QTc INTERVAL
Another speculative conclusion is drawn from a study performed when comparing SIDS cases and the precondition of arrhythmia: irregularity in the heartbeat . This study provided evidence of an association between an irregular cycle on the victim's ECG (an electrocardiogram) recording during the first days of life and the subsequent occurrence of SIDS.
The particular irregular cycle on the ECG in question is the prolonged QT interval, namely the interval between the Q wave and the T wave on the ECG. It is suspected that such a prolonged QT interval could be related to the dysfunction in the involuntary signals that are associated with the cortical arousal process, which is the primary finding in SIDS.
The Circumstances Under Which SIDS Occurs
Three conditions are found to occur in SIDS case studies:
1)Prenatal vulnerability: such as genetic or physiological pre-condition.
2)A critical developmental period between 6 weeks and 6 months and
3)An external unfavorable condition: such as head covering or prone sleep position.
PRONE VS SUPINE POSITION15 AND SIDS
Since 1994, public awareness campaigns throughout the Western world have led to an over 50% reduction in post-neonatal mortality and the frequency of SIDS. This reduction in mortality has been mainly attributed to the “Back To Sleep” campaign to raise awareness against the prone sleeping position, where the baby is put to sleep on their belly with the face to their side.
Scientists have proven that babies with genetic or physiological preconditions stated above are at high risk of SIDS when sleeping in prone position. Prone position is seen to impact the cortical arousal and sub-cortical activation in these victims.
Compared with the supine position, prone sleep position decreased the frequency of cortical arousal in REM sleep. The frequency of sub-cortical activation showed no significant differences between prone and supine positions. Sleeping on the belly (prone sleep position) decreased the frequency of waking up (cortical arousal) but did not change the frequency of wake-up signals (sub-cortical activation).
This means that when sub-cortex would send a wake-up signal to the cortex, the cortex would not respond by waking up - the main condition in SIDS victims.
AMBIENT TEMPERATURE16 AND SIDS
Parents have been warned against overdressing their babies for the risk of overheating, which is thought to be a condition leading to SIDS. Victims of SIDS were found unusually warm covered in sweat. This alerted experts to cautioning parents about a possible relation.
Here we will learn what the studies teach us about overheating, what parts of the body is impacted by overheating and how does that relate to SIDS.
Studies show that an increase in body temperature is accompanied by a decrease in oxygen levels below basal oxygen saturation (lowest permissible levels of oxygen in the blood). Increase in body temperature was also accompanied by higher occurrences of a drop in saturation levels of oxygen. It is known that such a drop in oxygen saturation is associated with central apnea during REM sleep. It was also seen that elevation in ambient (room) temperature and the corresponding mild core temperatures led to significant changes in cardiac and respiratory control systems. It is implied that such changes could attribute the sudden death to elevated ambient temperature.
Prenatal and Post Natal Smoking and SIDS
Smokong is postulated to impair infants’ brain and lung functions especially with exposure during fetal life pre-birth. This makes smoke exposed infants twice at risk of death by SIDS.
Swaddling and SIDS
Swaddling in supine position, sleeping on the back, is seen to reduce the risk of SIDS, however swaddling in the prone position is seen to increase the risk of SIDS.
The theory behind these statements is this: An immobilized infant can't crawl into dangerous asphyxiating (that compromising normal breathing) environments. Also, swaddling prevents infants from pulling bedding over their heads by kicking or pulling by hands. Both are risk factors of accidental suffocation.
On the contrary, in the case of prone sleepers, head lifting and turning to avoid an asphyxia environment are hindered when the arms are restrained at the baby's side rather than positioned beside the infant's head. It is also maintained that an infant that is sick or with a cough should not be swaddled as it hinders the ability to draw air into the lungs in the event of a forceful cough.
In summary, it should be noted that currently there is insufficient evidence that infants swaddled while supine are at any increased risk for SIDS. All in all, it would appear that the advantages of swaddling supine sleeping infants outweigh the risks, if any.
Sleep Maturity From 6 Weeks to 6 Months
Significant changes occur in sleep-awake mechanisms, breathing and involuntary controls in an infant between birth and 6 months. Infant’s sleep-awake pattern matures rapidly during this period. By 3 months of age, the proportion of rapid eye movement REM sleep begins to diminish and is replaced by NREM period.
With age there is also maturation of the ability of arousal from sleep. Between 0-6 weeks reflexes are seen to play a more dominant role in the arousal from sleep. After the first 6 weeks, there is a shift to a more deliberate voluntary behavior. During this shift the infant’s style of response undergoes a period of disorganized activity. According to the Handbook of Clinical Neurology, this period introduces a level of vulnerability.
In the event of obstruction in nasal passageway 83% of infants less than 6 weeks old were able to establish an oral passage way whereas only 54% of 6-week olds were able to do the same. This loss of reflexive behavior could be a risk factor if the voluntary responses are not already developed.
Can SIDS be Prevented?
The simple answer is no, SIDS cannot be completely prevented. However the risk of SIDS can be reduced by following safe sleep habits such as, not prone sleeping, not exposing an infant to second hand smoke, prohibiting smoking or drug abuse during pregnancy, lightly clothing the infant and controlling ambient temperature to 65-70oF.
Very few cases of SIDS were seen where there was use of a pacifier especially when used for sleep and when the mother were breastfeeding. The reasons for this reduction are unknown.
We hope this article sheds some light on the reasons behind some of the suggestions made to reduce the risks or SIDS and at the same time busts some myths around use of some products.
Please note that we have simply brought forth research findings from references noted below. This article is a summary of these references. It is by no means an independent medical paper resulting from independent study performed by individuals in the medical field.
References
(1--) The nature of arousal in sleep – Sept. 2003
11 Peterson DR (1988) Clinical implications of sudden infant death syndrome epidemiology. Pediatrician 15:198–203.
12 Distinguishing SIDS From Child Abuse
13 Distinguishing terms such as Suffocation, Asphyxia from SIDS
15 REM sleep is also called paradoxical sleep or active sleep. During REM sleep the brain waves emitted seem contradictory: although you are sleeping, your brain waves look at lot like what can be recorded when you are fully awake. The 4 different stages of sleep (NREM Stages 1-2-3, REM Sleep)
16 Spontaneous Arousability in Prone and Supine Position in Healthy Infants

